Kennebec Region Health Alliance
Promoting Healthy Communities Since 1997

DYSPEPSIA
Author: MaineGeneral Gastroenterology
Date: 4.27.16
Summary: Dyspepsia is defined as having one or more of the following symptoms:
- Epigastric pain or burning (classified as epigastric pain syndrome)
- Postprandial fullness (classified as postprandial distress syndrome)
- Early satiation (classified as postprandial distress syndrome)
- Approximately 25 percent of patients with dyspepsia have an underlying organic cause (see table).
- Functional dyspepsia (up to 75%): A diagnosis of functional dyspepsia can only be established after exclusion of other causes of dyspepsia.
Possible underlying causes of dyspepsia Peptic ulcer disease and H. Pylori infection
GERD
Biliary pain: gallstones, sphincter of Oddi dysfunction, functional gallbladder disorder
Chronic abdominal wall pain
Intra-abdominal cancer: Gastric or esophageal cancer, pancreatic cancer, hepatocellular carcinoma
Gastroparesis
Pancreatitis
Carbohydrate malabsorption
Medications: potassium, digitalis, iron, theophylline, antibiotics [especially ampicillin and erythromycin], NSAIDs, glucocorticoids, niacin, gemfibrozil, narcotics, colchicine, quinidine, estrogens, levodopa
Infiltrative diseases of the stomach (e.g., Crohn disease, eosinophilic gastroenteritis, sarcoidosis)
Metabolic disturbances (hypercalcemia, hyperkalemia)
Ischemic bowel disease, celiac artery compression syndrome, superior mesenteric artery syndrome
Systemic disorders (diabetes mellitus, thyroid and parathyroid disorders, connective tissue disease)
Intestinal parasites (Giardia, Strongyloides, Anisakis)
- History:
- GERD (heartburn, regurgitation, retrosternal burning pain) and NSAID use are common causes of dyspepsia
Alarm features
Age older than 55 years with new-onset dyspepsia
Family history of upper gastrointestinal cancer
Unintended weight loss
Gastrointestinal bleeding
Progressive dysphagia
Odynophagia
Unexplained iron deficiency anemia
Persistent vomiting
Palpable mass or lymphadenopathy
Incidental findings on imaging suggesting organic disease
- GERD (heartburn, regurgitation, retrosternal burning pain) and NSAID use are common causes of dyspepsia
- Examine for:
- Carnett’s sign: The presence of increased local tenderness during muscle tensing suggests the presence of abdominal wall pain.
- A palpable abdominal mass
- Lymphadenopathy (e.g., left supraclavicular or periumbilical in gastric cancer)
- Jaundice (e.g., secondary to biliary obstruction, liver metastasis)
- Pallor (secondary to anemia)
- Labs:
- CBC, LFTs, Lipase
Diagnostic strategies and initial management:
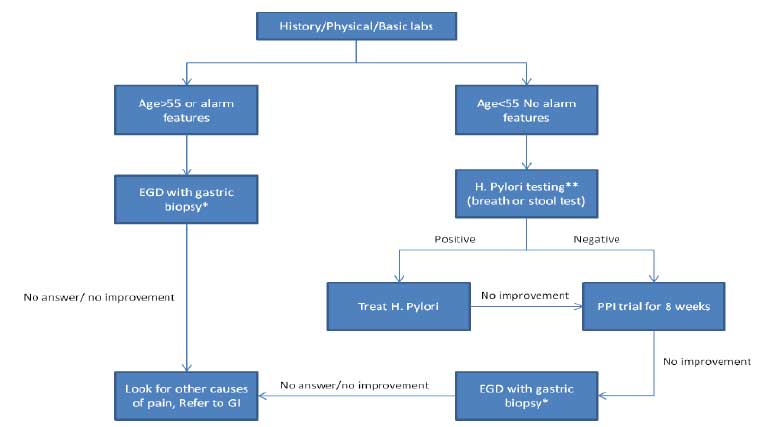
*5-biopsy Sydney System (lesser and greater curvature of antrum, lesser and greater curvature of body, incisura angularis) plus duodenal biopsy if indicated.
**Stool antigen assay preferred. Urea breath testing optional. Do not use serology testing. Test should be done 2-4 weeks (preferred 4 weeks) after stopping PPI, antibiotics, bismuth.
Notes:
- Endoscopy should be considered for patients in whom there is a clinical suspicion of malignancy even in the absence of alarm features.
- A negative endoscopy may reduce patient’s anxiety and increase patient satisfaction.
Practice Guidelines and Standard Processes Disclaimer
To promote the provision of efficient and effective healthcare services, Kennebec Region Health Alliance helps develop and disseminates practice guidelines for use by its member practices. Such guidelines are based upon various sources that KRHA believes to be reliable, which may include but is not limited to, guidelines from widely recognized professional societies, boards and colleges such as the American Medical Association (AMA). Practice guidelines are reviewed at least every two years and updated as necessary to reflect changes in medical practice.
These practice guidelines are not meant to express standards of care and should not be regarded as evidence of such standards. These Guidelines describe criteria for general operating practice and procedure and are for voluntary use. Guidelines are not a substitute for a physician’s or healthcare professional’s independent judgment.
Information on this website should not be relied on as an alternative to medical advice from a physician or other healthcare professional. If there are specific questions on any medical matter, a physician or healthcare professional should be consulted.